Next week is Macular Degeneration Awareness Week, an annual campaign initiated by Macular Disease Foundation Australia to raise awareness of the risk factors and symptoms of macular degeneration and to encourage all Australians at risk of the disease to have an eye test and macula check.
Macular Degeneration: What You Need to Know
From 23 to 28 May, we will be donating 10% of all earnings from MD patients to help the Foundation achieve its mission to reduce the incidence and impact of macular diseases in Australia. If you would like to make a private donation.
You may have seen the brochures and television advertisements asking you “Have you had your macula checked?” So what exactly is this ‘macula’ and what is ‘macular degeneration’?
Firstly, we need to understand some basic eye anatomy. The retina is the photosensitive layer of the eyeball, a bit like the film in a traditional camera, which has light-sensitive pigment cells called photoreceptors. The macula is a small area of the retina with the highest concentration of photoreceptors, providing us with our central vision, visual acuity (ability to detect fine detail) and colour vision. Another anatomical feature that is important in understanding macular degeneration is the Retinal Pigment Epithelium (RPE). This layer of the eye is situated outside the retina and ensures retinal health by providing nutrients such as oxygen and removing retinal metabolic waste products.
Macular Degeneration (MD) is a chronic and progressive eye disease in which the photoreceptors at the macula start to deteriorate and die due to the breakdown of the RPE. This causes a build-up of retinal metabolic waste that clinically appears as yellow spots, called drusen. There are two main forms of macular degeneration: commonly referred to as ‘dry’ and ‘wet’. To date, we still do not fully understand the cause of the disease and currently there is no cure.
The dry form, which makes up about 85% of moderate to advanced MD cases, is characterised by a slow, progressive loss of the RPE cells due to the build up of drusen at the macula[1]. This results in a gradual deterioration of the central vision. Diet and a special formulation of vitamins and high-dose antioxidants derived from the AREDS 1 and 2 studies, such as MacuTec Essentials or MacuTec Once Daily, have been shown to slow down the progression of MD in those with moderate to advanced MD in at least one eye[2,3]. The wet form, affecting about two-thirds of advanced MD patients, occurs when abnormal blood vessels grow underneath the macula. These vessels can spontaneously bleed, leading to a sudden loss of vision requiring immediate medical treatment, often with regular injections to shrink the blood vessels[1].
MD results in the loss of central vision and has the potential to severely impact our daily lives by affecting our ability to read, drive, recognise faces and discriminate fine detail. MD is the leading cause of legal blindness and low vision in developed countries. In Australia, approximately one in seven over the age of 50 have an element of MD and it contributes to 50% of legal blindness[4,5]. The main risk factors of developing MD are: age, family history of MD and smoking [1,6,7].
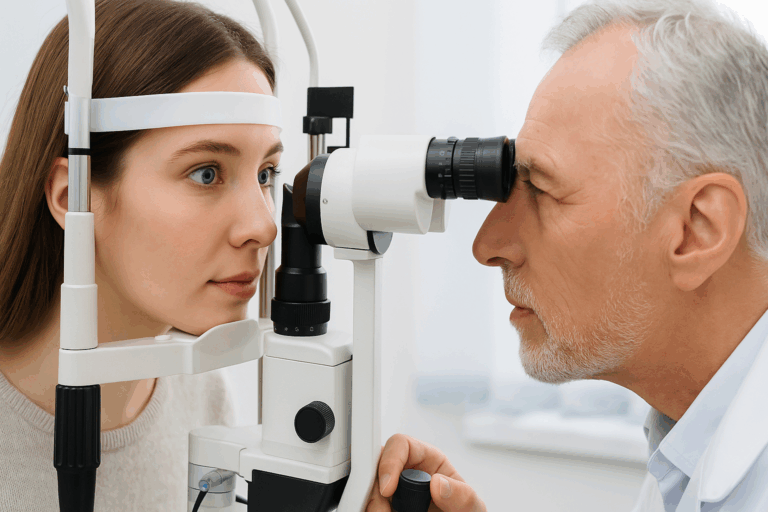
Your optometrist plays a very important role in diagnosing and managing MD as early detection and, if necessary, referral to an ophthalmologist is vital for a better visual outcome. Optometry Australia recommends a comprehensive eye examination at least every 2 years, and your optometrist may recommend more frequent visits if you are at a higher risk.
It is important to note that dry MD can convert to the wet form, which requires prompt treatment. This is why it is essential for all MD patients to monitor their macular closely with an Amsler Grid, and to see their eye health professional regularly. Additionally, optometrists help to improve the quality of life for MD patients by prescribing low vision aids and counseling about home environmental changes to maximise the use of their remaining vision.
Here are some ways to promote macular health[1,7]:
- Have your eyes and macula checked regularly by your optometrist.
- Abstain from smoking.
- Have a well-balanced diet including fresh fruit and vegetables (especially green leafy vegetables) daily, oily fish 2 to 3 times a week, handful of nuts a week, limit fat intake and high-GI carbohydrates.
- Exercise regularly and maintain a healthy body weight.
- Have adequate sun protection for your eyes.
If you have been diagnosed with macular degeneration, consult with your optometrist or ophthalmologist to see if supplements, such as those from the MacuTec range, are suitable for you.
Book an appointment for a thorough eye check-up or Call the Bondi clinic on (02) 9365 5047 or the Mosman clinic on (02) 9969 1600.
[1] Hampton T. Genetic Research Provides Insights Into Age-Related Macular Degeneration. JAMA. 2010;304(14):1541-1543.
[2] Age-Related Eye Disease Study Research Group. A Randomized, Placebo-Controlled, Clinical Trial of High-Dose Supplementation With Vitamins C and E, Beta Carotene, and Zinc for Age-Related Macular Degeneration and Vision Loss: AREDS Report No. 8. Arch Ophthalmol. 2001;119(10):1417-1436.
[3] The Age-Related Eye Disease Study 2 (AREDS2) Research Group. Lutein + Zeaxanthin and Omega-3 Fatty Acids for Age-Related Macular Degeneration: The Age-Related Eye Disease Study 2 (AREDS2) Randomized Clinical Trial. JAMA.2013;309(19):2005-2015.
[4] VanNewkirk MR, Nanjan MD, Wang JJ, Mitchell P, Taylor MD, McCarty CA. The prevalence of age-related maculopathy: The Visual Impairment Project. Ophthalmology 2000; 107: 1593-1600.
[5] Mitchell P, Taylor HR, Keeffe JE, Vu H, Wang JJ, Rochtchina E, Pezzullo LM. Vision Loss in Australia. Med J Australia 2005; 12: 565-568.
[6] Guymer RH, Chong EW. Modifiable risk factors for age-related macular degeneration. Med J Australia 2006; 184(9): 455-8.
[7] Macular Disease Foundation (www.mdfoundation.com.au/content/macular-degeneration-about).